Patient Resources
Get Healthy!
Health Care Plans Keep Allergy Rescue Injectors Pricey for Some
- July 15, 2022
- Ellie Quinlan Houghtaling
- HealthDay Reporter
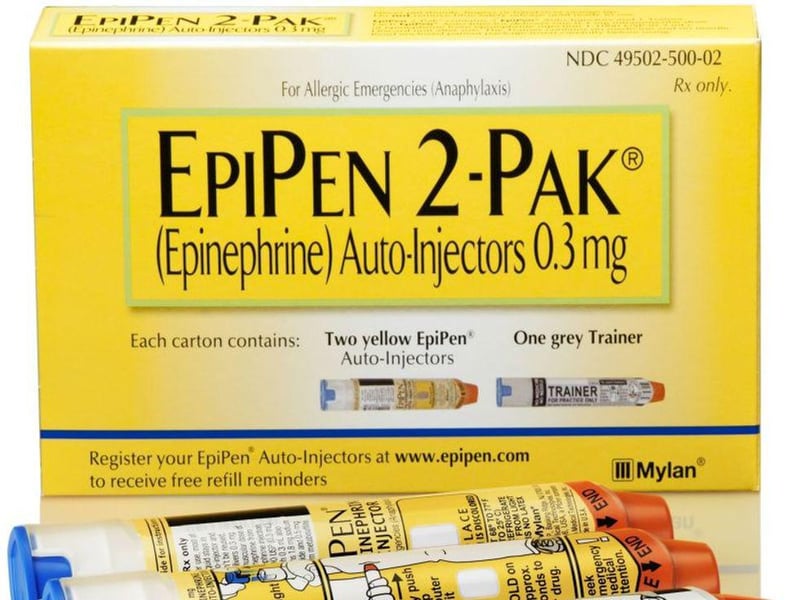
Despite now having more choices for lifesaving emergency allergy injectors like EpiPens, the cost is still proving prohibitively expensive for some, new research shows.
Even though most people are saving money with lower-priced alternatives after the cost of EpiPens shot up a few years ago, a significant minority of users -- people with high deductibles on their health insurance -- are still paying too much.
"Our findings suggest that the availability of lower-priced competitors did not solve the affordability problem for all patients who use epinephrine auto-injectors, particularly those covered by plans that require deductible and co-insurance payments for drugs," said lead study author Dr. Kao-Ping Chua. He's a pediatrician and health policy researcher at Michigan Medicine/University of Michigan.
The study examined 2015-2019 data from more than 657,000 children and adults through the IBM MarketScan Commercial Database, which houses claims data from 28 million Americans with employer-sponsored insurance.
The researchers' previous work on this topic, published in 2017, analyzed the amount that privately insured Americans paid every year for the EpiPen between 2007 and 2014. During this period, EpiPens were the only major epinephrine auto-injector available on the market. Not surprisingly, the study authors found out-of-pocket spending for the EpiPen doubled during that period, largely because the product's list price tripled.
But the new study focused on data from when new competitors to EpiPens were being introduced. Between 2015 and 2019, lower-priced generics such as Adrenaclick and Teva came to the market.
The authors found that the mean annual out-of-pocket spending for the auto-injectors peaked in 2016 at $116, but began to decrease when patients shifted to the less-expensive competitors. By 2019, annual out-of-pocket spending fell to $76, and 60% of patients paid $20 or less for the auto-injectors.
But even at the tail end of those years, 1 in 13 patients still paid more than $200 for the medicine. Among those patients, 62.5% were enrolled in high-deductible health care plans. These popular plans cover roughly 30% of privately insured Americans.
More than 63% of the patients paying over $200 each year were children, which researchers believe might be due to the fact that children typically need double the amount of medication than adults, as they need them both at home and at school.
"Our study shows patients can still pay a lot even if they use lower-priced epinephrine auto-injectors. To improve affordability for these patients, insurers could consider capping the out-of-pocket cost of non-branded auto-injectors," Chua said in a university news release. "Alternatively, the federal government could consider a federal cap similar to the one currently being discussed for insulin."
The findings were published July 11 in the Journal of General Internal Medicine.
More information
Visit the U.S. Food and Drug Administration for more on allergy relief for children.
SOURCE: University of Michigan, news release, July 12, 2022

